Lead Investigator
Areas of Impact
Overview
Opioids can assist in pain management, but can also lead to addiction and overdose. In a previous pilot of the current study, we reduced opioid prescribing doses by 11% through an intervention to increase adherence to opioid prescribing guidelines. As part of a larger project, our current intervention is implemented in 31 primary care clinics in two health systems serving the southern and northeastern areas of Wisconsin.
The Clinical Problem
Opioid misuse and abuse has become a significant public health problem in virtually all areas of the United States, including Wisconsin. This is particularly relevant during the COVID-19 pandemic, with preliminary data from the CDC suggesting a 16.4% increase in the number of drug overdose deaths in the first quarter of 2020 (compared to the first quarter of 2019).
Clinical guidelines for safer use of opioids were initially proposed in 2009, and have since evolved into the CDC’s widely publicized 2016 guidelines for opioid prescribing. The uptake of these guidelines has been variable across the U.S. healthcare system, and scholars have further documented the misapplication of guidelines, suggesting further attention is needed to balance the risks and benefits of opioids prescribed in primary care. Particularly during COVID-19, with projected increases in overdose deaths and the rise of telemedicine, implementation and adherence to prescribing guidelines is critical to meet the needs of patients struggling with chronic pain throughout Wisconsin.
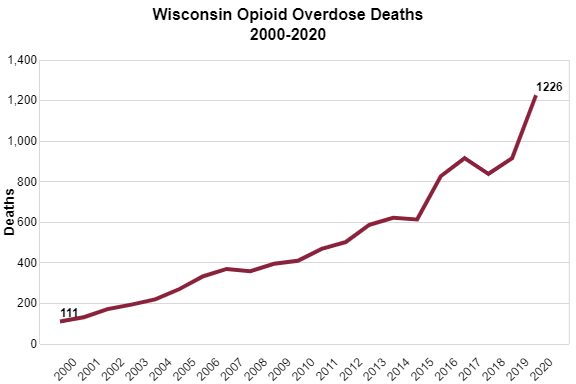
Source: Wisconsin Interactive Statistics on Health: https://www.dhs.wisconsin.gov/wish/opioid/index.htm
Our Response
Systems consulting: A multilevel approach
Clinical guidelines are often difficult to interpret for practitioners, and hard to implement system-wide. To assist in the uptake of clinical guidelines, University of Wisconsin researchers are implementing a novel and multiphase implementation strategy, called systems consultation.
“Clinical guidelines are often difficult to interpret for practitioners, and hard to implement. This is meant to be a model that potentially could be used nationwide.” — Andrew Quanbeck, PhD, Assistant Professor, UW-Madison Department of Family Medicine & Community Health
At the health system level, academic detailing includes quarterly educational meetings on the application of guidelines and monthly data reports to track best practices. At the clinic level, facilitators empower clinics to implement changes in their clinic workflows and increase adherence to opioid prescribing guidelines. Finally, at the prescriber level, physician coaches work with their colleagues to problem solve and consult in cases with individual patients, particularly those that may be at higher risk of developing addiction.

Results
Opioid doses fell by 11 percent at four clinics in the pilot study that paid special attention to urine drug testing and other monitoring of patients, while doses went up 8 percent at four other clinics not involved in the coaching program.
A clustered, sequential, multiple-assignment randomized trial (SMART trial) is currently underway that utilizes knowledge gained during the pilot to deliver an adaptive implementation strategy. The study works with 31 primary care clinics from two health systems statewide to more precisely reveal which elements of the implementation strategy are essential in different clinical settings, and how much it costs to implement these strategies. This will allow our research team to create a tailoring tool to help future clinics determine the most efficient and cost-effective methods of promoting clinical guideline adoption for opioid prescribing in primary care.
Lasting Impact
This research advances implementation science by demonstrating:
- a method for distilling clinical guidelines into a concise implementation guide.
- a blended implementation strategy, based on principles of systems engineering, that successfully put the guidelines into practice.
- a study design for testing multiphase implementation strategies and determining which combination of strategies may be most efficient and cost effective within different clinic contexts.
A randomized trial is being planned to use the knowledge gained during this study to deliver an adaptive implementation strategy. The randomized trial will seek to recruit 38 primary care clinics from three health systems statewide—UW Health, SSM Health/Dean Medical Group, and Bellin Health—to more precisely reveal which elements of the implementation strategy are essential in different clinic settings, enabling us to determine the most efficient methods of promoting clinical guideline adoption for opioid prescribing in primary care.
References
- CDC (2020). NCHS, National Vital Statistics System. Table 1. Percent of drug overdose deaths by quarter and demographic characteristics: United States 2019-Q1 through 2020-Q1.
- Dowell D, Haegerich T, Chou R. No Shortcuts to Safer Opioid Prescribing. N Engl J Med. 2019 Jun 13;380(24):2285-2287
- Jacobson N, Johnson R, Deyo B, Alagoz E, Quanbeck A. Systems consultation for opioid prescribing in primary care: a qualitative study of adaptation. BMJ Qual Saf. 2019 May;28(5):397-404.
Wisconsin Department of Health Services. Preventing and Treating Harms of the Opioid Epidemic: An assessment to identify geographic gaps in services, and a plan to address these gaps (Feb, 2020). - Quanbeck A, Almirall D, Jacobson N, Brown RT, Landeck JK, Madden L, Cohen A, Deyo BMF, Robinson J, Johnson RA, Schumacher N. The Balanced Opioid Initiative: protocol for a clustered, sequential, multiple-assignment randomized trial to construct an adaptive implementation strategy to improve guideline-concordant opioid prescribing in primary care. Implement Sci. 2020 Apr 25;15(1):26.
- Quanbeck A, Brown RT, Zgierska AE, Jacobson N, Robinson JM, Johnson RA, Deyo BM, Madden L, Tuan WJ, Alagoz E. A randomized matched-pairs study of feasibility, acceptability, and effectiveness of systems consultation: a novel implementation strategy for adopting clinical guidelines for Opioid prescribing in primary care. Implement Sci. 2018 Jan 25;13(1):21.
- Quanbeck A, Brown RT, Zgierska AE, Johnson RA, Robinson JM, Jacobson N. Systems consultation: protocol for a novel implementation strategy designed to promote evidence-based practice in primary care. Health Res Policy Syst. 2016;14(1):8.

