Lead Investigator
Resources
For more information, please contact Dr. Meghan Brennan at mbbrennan@wisc.edu
Areas of Impact
Overview
Approximately 2 million Americans develop a diabetic foot ulcer each year. Within 5 years of ulceration, over 50% die and 5% lose a limb. Diabetic foot ulcers cost the U.S. healthcare system $130 billion annually, require significant patient self-management in terms of daily wound care and ambulation restrictions, and can result in devastating function impact if a major (above- or below-knee) amputation is required. Patients often fear major amputation from diabetic foot ulcers more than death.
The Clinical Problem
Rural patients with diabetic foot ulcers currently face 50% higher odds of major (above-ankle) amputation and 40% higher odds of death than their urban counterparts, a health disparity identified by Dr. Meghan Brennan’s team and others. Over 70% of Wisconsin residents live in rural areas, making this a particularly important topic to address in our state.
Our Response
Identifying urban successes
There has been a recent surge in urban, integrated care teams for patients with diabetic foot ulcers. These teams bring together specialists in glycemic control, vascular disease, biomechanics, and infection to optimize wound healing. Dr. Brennan’s systematic review found that addressing these underlying factors in a timely, coordinated manner reduced major amputations by ~40%. Teams of multiple specialists worked side-by-side to optimize success. Many developed their own care algorithms and referral pathways to streamline this care. Integrated care teams have not been adapted to the rural setting, where specialists are scarce. They have also minimally engaged primary care providers, many of whom could significantly contribute to integrated care.
Understanding current collaboration for rural patients with diabetic foot ulcers
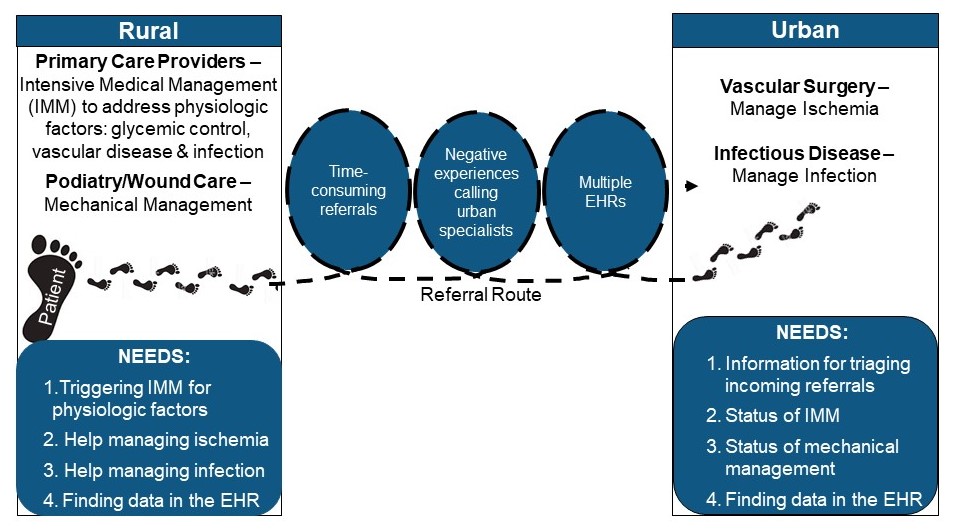
Dr. Brennan’s team identified significant barriers to collaboration between rural providers and urban specialists caring for rural patients with diabetic foot ulcers (quote text box). These included: time-consuming referral processes, negative experiences calling urban specialists, and difficulties communicating across multiple electronic health record systems (conceptual model). This qualitative work involved interviews with over 40 stakeholders, including rural providers, urban specialists, nurses, administrative support staff, patients and their caregivers. It was also the beginning of an ongoing partnership with the Rural Wisconsin Health Cooperative, an organization that represents 43 rural health systems across the state. The Cooperative provided feedback on how to prioritize the team’s findings to target with a subsequent intervention co-design.
“Where do I send someone with a diabetic foot ulcer that’s beyond my skill level? Maybe it’s not an emergency, but they need a higher level of care. For one patient, who’s on his fourth visit with me, I ended up admitting him, and he got amputated. It was really a sad outcome. I feel like if there was better coordination, it could have been prevented.” — A rural primary care provider
Care algorithm co-design
Dr. Brennan’s team are currently working with the Rural Wisconsin Health Cooperative to design a care algorithm and referral checklist for rural patients with diabetic foot ulcers. The pathway outlines management of the four physiologic factors addressed by integrated care: glycemic control, vascular disease, biomechanics, and infection. It is intended to be used by rural primary care providers and specialists. It also provides guidance on when to refer to urban specialists (typically vascular surgeons and infectious disease specialists), and what information to send in the referral packet.
Lasting Impact
Testing of the care algorithm and referral pathway in Rural Wisconsin Health Cooperative clinic sites throughout the state have begun as a way to address the rural disparity in major amputations and death. The testing will be the first initiative to close this gap. Dr Brennan’s team is implementing the algorithm and referral pathway in rural clinics and monitoring its effect on patient care.
Acknowledgements
Financial support for this work was provided by, a 2018 ICTR Pilot Award with support from NIH CTSA grant 1UL1TR002373, and the UW-Madison SMPH Wisconsin Partnership Program grant # 3086. To pursue this line of work, Dr. Brennan received a 2022 NIH-NIDDK R01 award (R01 DK132569-01), ICTR KL2 award (TR000428) and an AHRQ K08 award (PA-17-232).
Reference
Sutherland BL, Pecanac K, Bartels CM, Brennan MB. Expect delays: poor connections between rural and urban health systems challenge multidisciplinary care for rural Americans with diabetic foot ulcers. J Foot Ankle Res. 2020 Jun 16;13(1):32.

